What is a cornea?
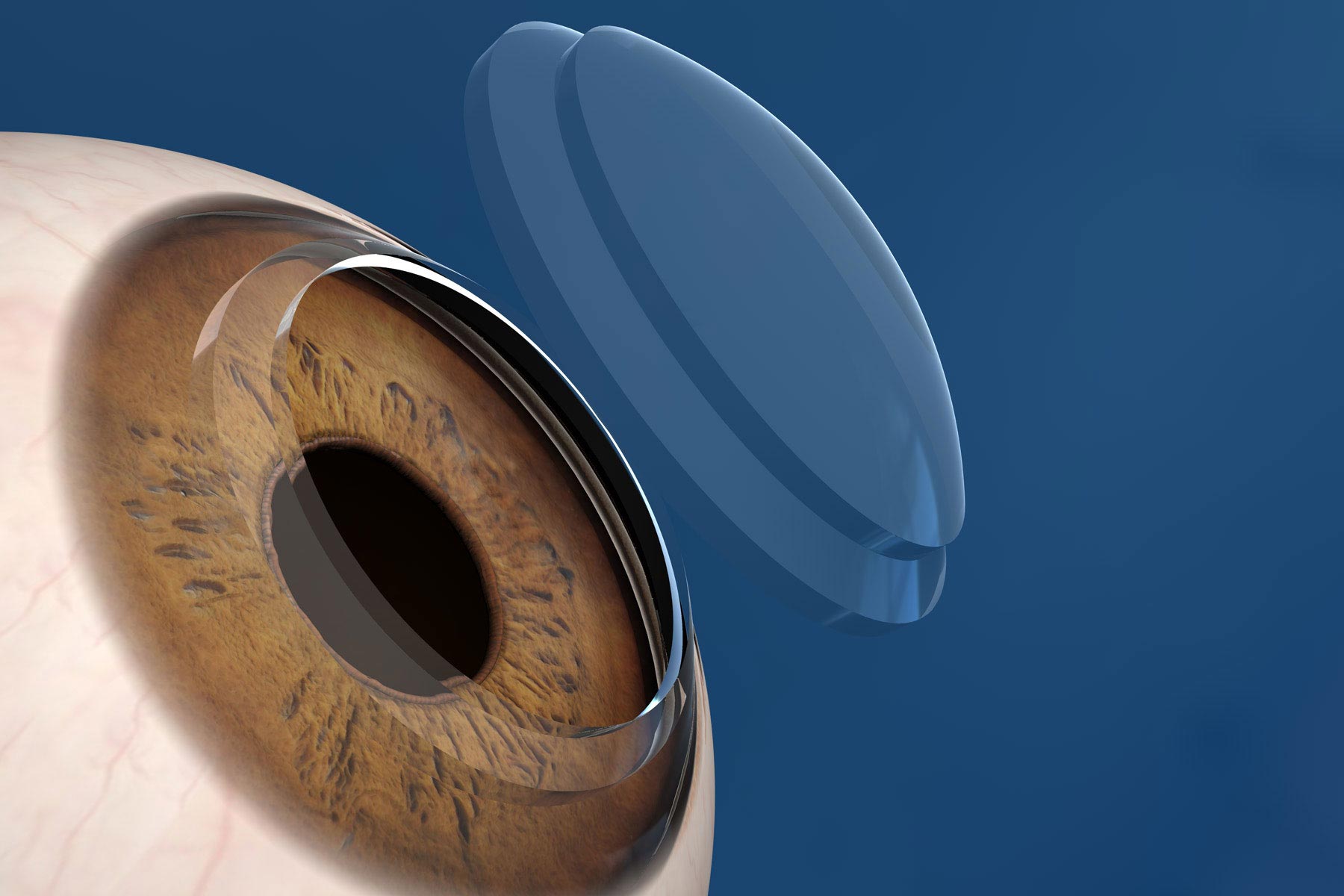
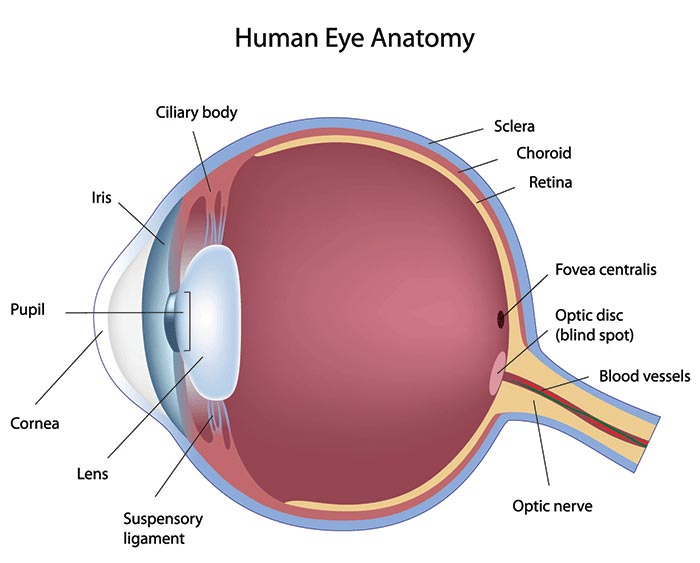
The cornea is the central part of the front of the eye through which we see. Normally, the cornea is smooth and transparent. However, injury, disease or certain medical conditions can make it cloudy or difficult to see through. Sometimes removing some or all of the cornea and replacing it with corneal tissue from an organ donor can fix this problem. This operation is called corneal transplantation. [view photos]
Is it safe to receive donated corneal tissue? It is safe to receive donated corneal tissue. The medical history of every organ donor is reviewed carefully, and blood tests are performed to check for infections prior to corneal transplantation. If there is any doubt about the safety of corneal transplantation, the donated tissues are used for medical research instead of being transplanted into a patient's eye.
Why do people need a corneal transplantation?
There are several reasons for performing corneal transplantation:
- External trauma: Sometimes an injury might damage the cornea so severely that it might not heal correctly. The cornea plays an important role in vision, so even a small corneal injury can greatly reduce vision. Corneal transplantation might be recommended to restore vision, or in severe cases, it might be warranted to close to defect ensued.
- Internal Trauma: Some people experience corneal swelling and clouding after intraocular surgery like cataract surgery due to a surgically induced injury to the cells lining the back of the cornea (corneal endothelium). This is known as pseudophakic bullous keratopathy and is a common reason for corneal transplantation.
- Infections & certain medical conditions: Some infections of the eye can cause damage to the cornea that will not heal. Bacterial infections (whether contact lenses-induced or not), Herpes virus infections, etc...
- Inherent corneal diseases: There are also certain medical conditions that make the cornea very thin or cloudy, or cause other problems that can only be treated by replacing the cornea, partially or totally. The following are common cornea diseases that might require transplantation: Keratoconus is a condition where the cornea becomes thin and weak, and eventually bulges outward in a cone-like shape, causing severe vision problems. Vision with glasses might not be satisfactory, and treatment modalities can include rigid gas permeable contact lenses ("hard lenses") or hybrid contact lenses, ring segment implants insertion (INTACS SK, Ferrarings, or Kerarings), corneal cross-linking, and corneal transplantation, as a last resort.
[Link: Keratoconus overview on doctor awwad.com]
Fuch’s Dystrophy is a genetic predisposition for a cornea to progressively imbibe water as we age due to a defect in the cells lining the back of the cornea (endothelial cells), resulting in a decrease in vision due to loss in overall optical quality and transparency of the cornea. This disease is often silent early in life, and it starts manifesting slowly with age. Often, an endothelial transplantation is required (DMEK & DSEK).
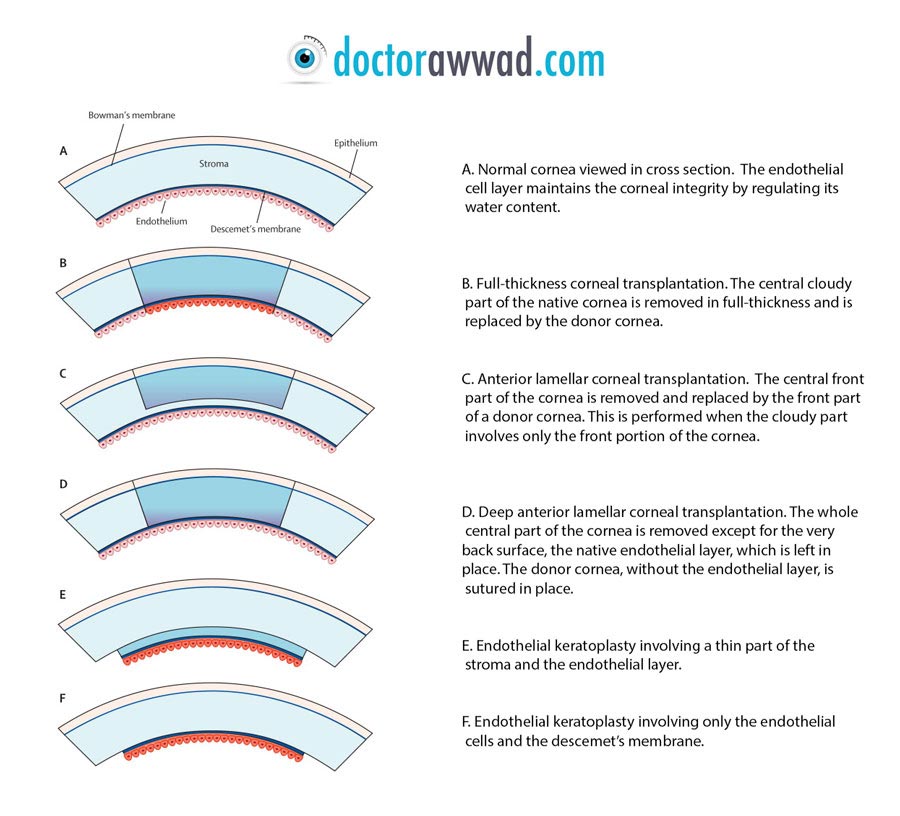
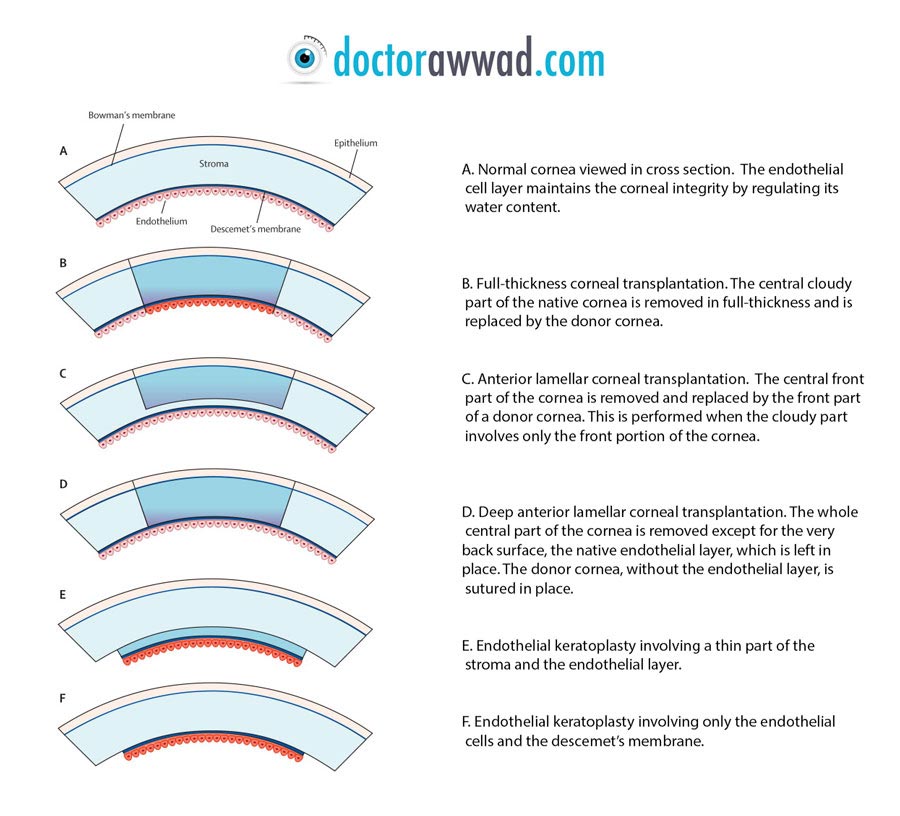
Full thickness corneal transplantation (Penetrating Keratoplasty) Corneal transplantation can be done under general anesthesia; that is, with the patient "asleep." Local anesthetic, in which the patient is awake but does not feel the procedure, also can be used. A portion of the cornea is removed using scissors and a special instrument called a trephine, which works like a tiny circular cookie-cutter. This leaves an opening in the patient's cornea. Other techniques make use of the femtosecond laser to perform the initial circular cut. A similarly sized trephine is used to cut a section from the donor cornea. This section of corneal tissue is placed into the opening in the patient's cornea and fastened with very small stitches. After surgery, it is important not to put any pressure on the eye. It is best not even to touch or rub anywhere near the eye, and a transparent plastic eye shield is used to pitch the eye overnight for a few months. Wearing glasses or sunglasses will also help protect the eye. Steroids and antibiotics eye drops are prescribed to help the eye heal and prevent infection. Those drops are be used for several months after a corneal transplantation. Without these medications, the eye might reject the transplanted corneal tissue, or develop infection. vision is expected to improve slowly, but optimal vision might not be attained before 6 months to a year after surgery. Suture removal can be performed at 10-12 months to improve vision of need be.
If the main problem is in the back part of the cornea (weak cell layer not pumping water out of the cornea), then an endothelial transplantation can be performed, instead of a full thickness corneal transplantation. The advantages include a less invasive surgery, less risk of rejection, and a quicker visual recovery. A cornea from a human donor is still needed. The donor cornea is sliced, and only the back part of the donor cornea is used. The patient's cornea is not cut, but its inner layer (endothelium) is stripped, and the back slice of the donor cornea, containing a healthy endothelium, is inserted into the patients eye and attached to the back side of the donor (recipient) cornea with the help of an air bubble, which has as a function to exert a constant upward pressure on the donor corneal tissue to adhere to the patient's cornea. The whole procedure is performed through a tiny corneal incision, and is usually performed under local anesthesia.
When the front portion of the cornea is affected, with sparing of the back portion or back surface, only the front portion can be excised and replaced with the front portion of a cadaveric graft. Examples of potential candidates are some patients with keratoconus and superficial scars that are deep enough to make them ineligible for laser removal (PTK). The procedure is called anterior lamellar & deep anterior lamellar keratoplasty, depending on the extent of the transplantation depth.
The majority of the corneal transplantations done in patients with keratoconus, Fuch's dystrophy and endothelial dysfunction, corneal scars and most types of corneal diseases are successful. The operation is less successful in eyes with a corneal infection or severe injury such as a chemical burn. In a small number of cases, the new corneal tissue is rejected by the body’s immune system even though the operation was successful and all medications were taken correctly. In young keratoconus patients, the risk of rejection over 5-10 years seems to be around 5 %. Additionally, the cornea might fail to survive or “take” in its new medium and won’t function, necessitating another transplantation procedure. In total or partial corneal transplantation, Some corneas (around 8%) might harbor high amount of correction (e.g. myopia, hyperopic, and regular astigmatism) or appreciable irregular astigmatism and might necessitate fitting with rigid gas permeable contact lenses (hard lenses), or hybrid lenses. Some patients might develop high eye pressure during the course of the postoperative follow-up and might need to be treated with pressure lowering eye drops. In some condition, this condition can become chronic (glaucoma), necessitating permanent use of the pressure lowering medications.
Postoperative instructions
After corneal transplantation, patients should avoid rubbing their eyes at all times. They are instructed to protect their operated eye with polycarbonate eye glasses or eye shield, as well as use a protective transparent eye shield during sleep for at least one month. Water should not come in contact with the eyes for one week, and swimming should be avoided for at least one month. Patients are usually instructed to maintain low-key social and work activities for about one week, after which patients can resume normal daily activity. Smoking should preferably be avoided for the first week. The best way to avoid problems after corneal transplantation is to follow the doctor's advice, including using all medications as recommended and keeping all follow-up appointments. Medication will include antibiotic and steroid containing eye drops, which will be tapered slowly over the course of several months. Depending on the type of corneal transplantation, corneal stitches are removed anytime from several months to up to several years after surgery.
Visual expectation
Vision will be most likely blurry initially after corneal transplantation, however it should start to improve gradually over the next several weeks to months after the procedure. Depending on the type of transplantation performed and on patient’s individual variability, full visual recovery might take months and sometimes more than a year. It is not unusual for the operated eye to have suboptimal vision for several months. Later in the follow-up period, removing one or several corneal stitches in a staged approach based on corneal topography might dramatically improve vision. Eyeglasses, and sometimes contact lenses, are often needed to attain optimal vision. Laser vision correction and implantable contact lenses can be performed to enhance and rehabilitate vision when needed.
Alternative to donated corneal tissue? In special situations, like some types of chemical burns or repeatedly failed or rejected corneal transplantations, a special type of synthetic transparent prosthesis can be accommodated in the center of the human cornea. An example of the available synthetic prostheses is the Boston Kpro implant.